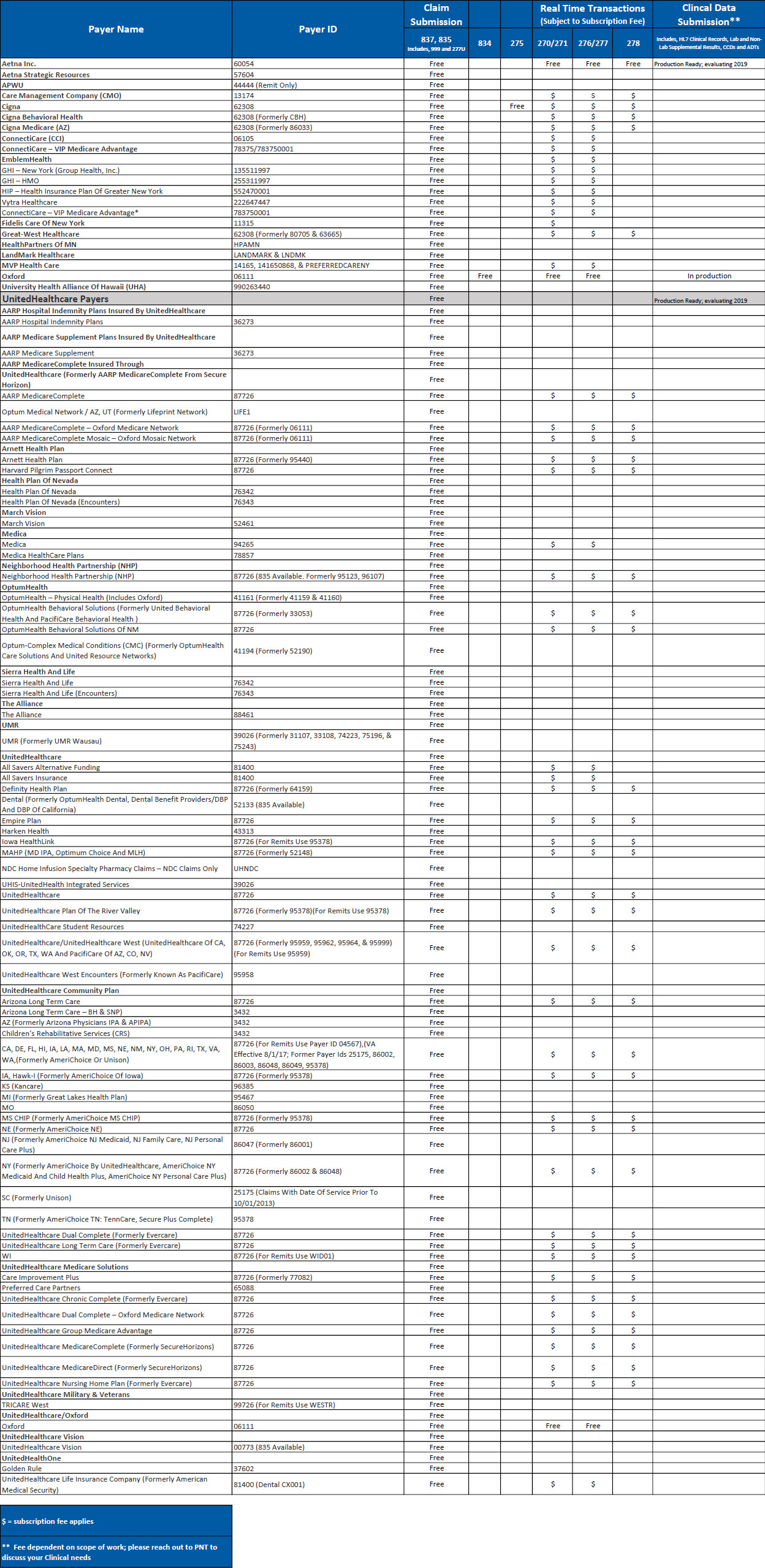
In the ever-evolving world of healthcare administration, staying informed about payer updates and changes is crucial for smooth operations and accurate claim processing. Medical billers, coders, and healthcare providers rely on timely notifications to ensure they are submitting claims correctly and receiving prompt reimbursement. These updates often involve intricate details such as payer IDs, which serve as unique identifiers for insurance companies. When these IDs shift, it can trigger a cascade of adjustments across billing systems and workflows.
Imagine the intricate dance between a doctor’s office and an insurance company. Patient information, diagnoses, and procedures all have to be meticulously documented and translated into standardized codes. These codes are then bundled into a claim and sent off to the payer for review and payment. The payer ID acts as the key that unlocks the right mailbox, ensuring the claim reaches the correct destination within the insurance company’s vast network.
Therefore, any alteration to a payer ID necessitates a careful and coordinated response. Healthcare providers must update their billing software, inform their staff, and potentially revise their internal processes. The goal is to avoid claim rejections, payment delays, and unnecessary administrative burdens. The process requires vigilance and precision to maintain the financial health of healthcare organizations.
The healthcare landscape is constantly shifting. New regulations are enacted, insurance plans are updated, and payers refine their internal systems. The changes may be minor adjustments to claim formats or significant overhauls of entire billing platforms. Regardless of the scope, healthcare providers must adapt quickly and effectively to stay ahead of the curve.
Recently, there was an announcement regarding a significant change that would impact healthcare providers. A change concerning HealthPartners, one of the major players in the healthcare insurance industry. The buzz surrounded a scheduled update to their payer ID. But information has been provided, that the HealthPartners Payer ID Change *DELAYED, giving providers some breathing room.
Understanding the Initial Announcement
Payer ID Changes: A Common Occurrence
Payer ID changes are not uncommon in the healthcare industry. They occur for various reasons, including mergers and acquisitions, system upgrades, or internal restructuring within insurance companies. When a payer ID changes, it means the unique identifier used to electronically submit claims to that specific payer has been altered.
The consequences of submitting claims with an incorrect or outdated payer ID can be significant. Claims might be rejected outright, leading to delays in payment and increased administrative costs. In some cases, claims might be misdirected to the wrong payer altogether, further complicating the reimbursement process.
Healthcare providers rely on accurate payer information to ensure timely and efficient claim processing. Many different sources of information, are constantly monitored in order to react to an upcoming change such as a payer ID update. Implementing a payer ID change involves a series of steps to minimize disruption. Medical billing software must be updated, staff must be trained on the new procedures, and internal workflows must be adjusted to accommodate the change.
Staying informed about payer ID changes is an ongoing process. Healthcare providers must regularly monitor announcements from insurance companies and other industry sources to stay abreast of the latest developments. Medical billing software vendors often provide updates and alerts to help their clients manage payer ID changes effectively.
The initial announcement of the HealthPartners Payer ID Change *DELAYED caused a stir, prompting healthcare providers to prepare for the update. However, with the subsequent delay, providers now have an opportunity to review their processes and ensure they are fully prepared for the eventual change.
The Anticipated Impact on Healthcare Providers
The initial announcement of the HealthPartners payer ID change had many healthcare providers scrambling to update their systems. This involved checking with their clearinghouses, and software vendors to ensure a smooth transition. The anticipated impact included the potential for claim rejections, payment delays, and increased administrative burden. These challenges arise from the need to meticulously update billing systems and processes to reflect the new payer ID.
One of the most significant concerns was the potential for disruption to cash flow. Delays in claim processing can directly impact the financial health of healthcare organizations, especially smaller practices and clinics that rely on timely reimbursement. This financial strain can affect their ability to provide quality care to patients. Proper preparation is key.
Furthermore, the need to update billing systems and train staff requires time and resources, diverting attention from other important tasks. Some healthcare providers would even need to contact all their clients to resubmit information, which takes even longer.
Providers also faced the challenge of communicating the change to patients, particularly those with HealthPartners insurance. Ensuring patients understand the update and its potential impact on their billing statements is crucial for maintaining good patient relations.
The initial announcement emphasized the importance of proactive communication and preparation to minimize disruption. However, the subsequent delay in the HealthPartners Payer ID Change *DELAYED has provided a buffer period, allowing providers to better prepare and refine their processes.
Reasons Behind the Delay
System Integration Challenges
One of the primary reasons for delaying a payer ID change often lies in the complexities of system integration. Healthcare organizations and insurance companies rely on sophisticated software systems to manage billing, claims processing, and other administrative functions. When a payer ID changes, it can require extensive modifications to these systems to ensure seamless communication and data exchange.
Integrating a new payer ID across multiple systems can be a time-consuming and resource-intensive process. Each system must be carefully tested to ensure it is correctly processing claims with the new ID. Any errors or inconsistencies can lead to claim rejections, payment delays, and other administrative headaches.
Sometimes the system integration may not go as planned. Unexpected glitches or technical difficulties can arise, requiring additional time and effort to resolve. In some cases, it might be necessary to postpone the payer ID change to allow for thorough testing and troubleshooting.
In the case of HealthPartners, the delay in the payer ID change may be due to unforeseen challenges encountered during system integration. The organization may be working diligently to address these issues and ensure a smooth transition for healthcare providers. Delaying the HealthPartners Payer ID Change *DELAYED to the necessary extent, allows all issues to be resolved, which minimizes disruption.
Patience and understanding are essential during this time. Healthcare providers should continue to monitor announcements from HealthPartners and other industry sources for updates and guidance.
Ensuring Data Accuracy and Integrity
Data accuracy and integrity are paramount in the healthcare industry. Any errors or inconsistencies in patient information, diagnoses, or billing codes can have serious consequences. When a payer ID changes, it is crucial to ensure that all data is accurately transferred to the new system.
Data migration can be a complex and challenging process. It requires careful planning, thorough testing, and meticulous attention to detail. Errors in data migration can lead to claim rejections, payment delays, and even compliance issues.
To minimize the risk of data errors, insurance companies often conduct extensive testing and validation before implementing a payer ID change. This may involve running test claims, reviewing data samples, and comparing results to ensure accuracy. These steps help to verify that the new system is correctly processing claims and that all data is intact.
HealthPartners likely delayed the payer ID change to ensure that data accuracy and integrity are not compromised. The organization may be taking extra precautions to validate data and prevent errors from occurring. That allows them to be confident in the HealthPartners Payer ID Change *DELAYED before implementing it.
Healthcare providers should take this opportunity to review their own data and ensure it is accurate and up-to-date. This will help to minimize the risk of claim rejections and payment delays when the payer ID change eventually goes into effect.
Steps to Take During the Delay
Review and Update Billing Systems
The delay in the HealthPartners Payer ID Change *DELAYED provides a valuable opportunity for healthcare providers to review and update their billing systems. This includes checking with clearinghouses, software vendors, and other relevant parties to ensure that all systems are prepared for the eventual change.
Start by contacting your clearinghouse to confirm that they are aware of the delay and that they have updated their systems accordingly. Also, inquire about any specific steps you need to take to ensure a smooth transition.
Next, contact your medical billing software vendor to verify that your software is compatible with the new payer ID. If necessary, request any updates or patches to ensure that your system is up-to-date.
It’s also a good idea to review your internal billing processes and identify any areas that might need to be adjusted to accommodate the payer ID change. This may involve updating forms, revising workflows, or retraining staff.
By taking these proactive steps, you can minimize the risk of claim rejections and payment delays when the HealthPartners payer ID change eventually goes into effect.
Communicate with Staff and Patients
Effective communication is essential for managing any change in the healthcare industry. The delay in the HealthPartners payer ID change presents an opportunity to communicate with staff and patients about the upcoming update and its potential impact.
Start by informing your staff about the delay and explaining the reasons behind it. Emphasize the importance of staying informed and being prepared for the eventual change. Provide them with any relevant updates or guidance from HealthPartners or other industry sources.
Next, consider communicating with your patients, especially those with HealthPartners insurance. Explain that there was an adjustment that providers need to be updated on. Assure them that you are taking steps to ensure a smooth transition and that there should be no disruption to their care.
You might want to post a notice in your waiting room, send out an email, or include a message on your website. Providing clear and concise information can help to alleviate any confusion or anxiety among your patients.
Open communication will foster trust and cooperation, ensuring a seamless experience for everyone involved. Delaying the HealthPartners Payer ID Change *DELAYED means that more people can be properly notified and prepared.
Best Practices for Managing Payer ID Changes
Establish a Proactive Monitoring System
One of the best ways to manage payer ID changes effectively is to establish a proactive monitoring system. This involves regularly monitoring announcements from insurance companies, clearinghouses, and other industry sources to stay abreast of the latest developments.
Designate a staff member or team to be responsible for monitoring these sources and identifying any potential payer ID changes. They should track announcements, review updates, and disseminate information to the appropriate personnel within your organization.
Consider subscribing to email alerts or newsletters from insurance companies and clearinghouses. These sources often provide timely notifications about payer ID changes and other important updates.
Also, encourage your staff to report any suspected payer ID changes they encounter during their daily work. This can help to identify potential issues early on and prevent claim rejections.
By establishing a proactive monitoring system, you can stay ahead of the curve and ensure that your organization is prepared for any payer ID changes that may arise. Making the HealthPartners Payer ID Change *DELAYED easier to catch.
Implement a Standardized Update Process
To ensure consistency and accuracy, it is essential to implement a standardized update process for managing payer ID changes. This involves developing a clear set of procedures for updating billing systems, training staff, and communicating with patients.
Create a checklist of tasks that need to be completed whenever a payer ID changes. This might include updating billing software, revising forms, retraining staff, and notifying patients.
Assign responsibility for each task to a specific individual or team. This will help to ensure that all tasks are completed in a timely and efficient manner.
Document the update process and make it readily available to all staff members. This will help to ensure that everyone is following the same procedures and that no steps are missed.
Regularly review and update the standardized update process to ensure that it remains effective and up-to-date. This will help to minimize the risk of errors and ensure that your organization is always prepared for payer ID changes.
Potential Future Scenarios
A Revised Implementation Date
While the initial HealthPartners payer ID change has been delayed, it is highly likely that a revised implementation date will be announced in the future. Healthcare providers should remain vigilant and continue to monitor announcements from HealthPartners and other industry sources.
When a revised implementation date is announced, be prepared to act quickly. Update your billing systems, train your staff, and communicate with your patients about the upcoming change. Don’t let the delay cause complacency; use the time to prepare even more thoroughly.
Keep in mind that the revised implementation date may be subject to change if unforeseen circumstances arise. Be flexible and adaptable, and be prepared to adjust your plans accordingly. You never know if there will be a HealthPartners Payer ID Change *DELAYED yet again.
The key is to stay informed and be proactive. By staying on top of the latest developments, you can minimize the risk of disruption and ensure a smooth transition when the payer ID change eventually goes into effect.
The delay in the HealthPartners payer ID change provides a valuable opportunity for healthcare providers to prepare for the eventual update. By taking proactive steps to review and update billing systems, communicate with staff and patients, and establish a standardized update process, healthcare providers can minimize the risk of claim rejections and payment delays. This allows you to be extra diligent, ensuring that when the new implementation date hits, it’s smooth sailing from there.
Further Delays or Modifications
In the ever-changing landscape of healthcare administration, it is possible that further delays or modifications to the HealthPartners payer ID change could occur. While this is not the ideal scenario, it is important to be prepared for such possibilities.
If further delays are announced, don’t be discouraged. Use the additional time to refine your processes, conduct further testing, and ensure that your systems are fully prepared for the eventual change. It is not ideal, but more time to properly execute is invaluable.
If modifications to the payer ID change are announced, carefully review the details and make any necessary adjustments to your systems and procedures. Stay connected with the HealthPartners so you always know what the latest updates are.
Remember, flexibility and adaptability are key. By being prepared for potential changes and adjusting your plans accordingly, you can minimize the risk of disruption and ensure a smooth transition, regardless of what the future holds. Keep your eyes peeled to avoid another HealthPartners Payer ID Change *DELAYED announcement.
As a healthcare provider, you’re constantly having to adapt and overcome challenges. Being vigilant will help with any challenges in the future.
Conclusion
The HealthPartners Payer ID Change *DELAYED is a temporary situation, and the eventual implementation will require careful preparation and execution. By understanding the reasons behind the delay, taking proactive steps to update your systems and processes, and implementing best practices for managing payer ID changes, you can minimize disruption and ensure a smooth transition.
This delay serves as a reminder of the dynamic nature of healthcare administration and the importance of staying informed and adaptable. Proactive preparation is key to navigating these changes successfully.
We encourage you to explore our other articles for more insights and guidance on navigating the complexities of healthcare billing and administration. Stay informed, stay prepared, and stay ahead of the curve!
- The HealthPartners Payer ID Change has been delayed.